[Newsletter] 他氟前列素治疗青光眼和高眼压症的短期疗效与安全性研究 |
您所在的位置:网站首页 › 眼压iop和ciop › [Newsletter] 他氟前列素治疗青光眼和高眼压症的短期疗效与安全性研究 |
[Newsletter] 他氟前列素治疗青光眼和高眼压症的短期疗效与安全性研究
|
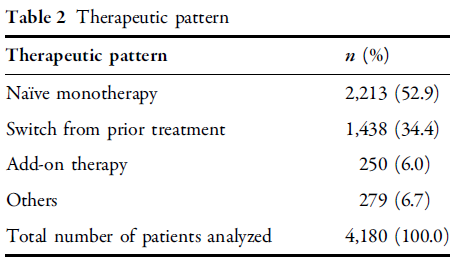
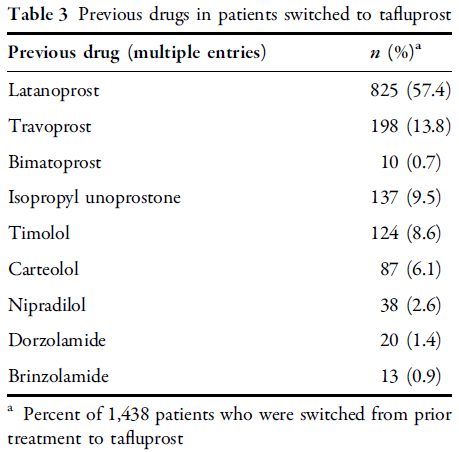
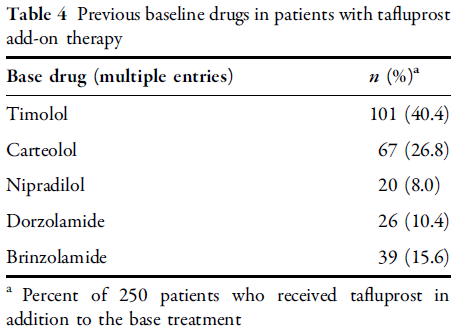
治疗方案 对患者使用的治疗方案见表2,包括52.9%患者为他氟前列素首次单药治疗,34.4%患者为替换为他氟前列素治疗,以及6.0%患者为附加治疗,他氟前列素替换治疗前的用药情况见表3,附加治疗前的用药情况见表4。
表2 治疗方案
表3 他氟前列素替换治疗前的用药情况
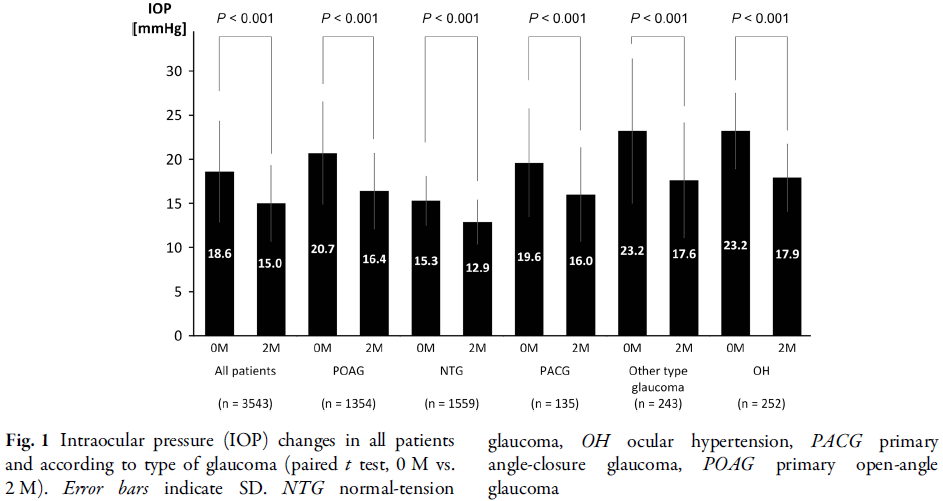
表4 附加治疗前的用药情况 0 3 降眼压作用 所有受分析患者基线平均眼压为18.6 ± 5.7 mmHg,2个月后为15.0 ± 4.3 mmHg,显著下降3.6 ± 4.5 mmHg。各类型青光眼IOP均显著下降,POAG下降4.3 ± 5.2 mmHg,NTG下降2.4 ± 2.5 mmHg,PACG下降3.6 ± 5.3 mmHg,其他类型青光眼下降5.6 ± 7.1 mmHg,OH下降5.3 ± 4.8 mmHg(图1)。各类继发性青光眼IOP也显著降低,假性剥脱性青光眼降低6.0 ± 7.0 mmHg,葡萄膜炎继发性青光眼降低7.7 ± 8.0 mmHg,新生血管性青光眼降低3.2 ± 5.2 mmHg(图2)。
图1 所有患者和按青光眼类型分类患者眼压(IOP)变化情况
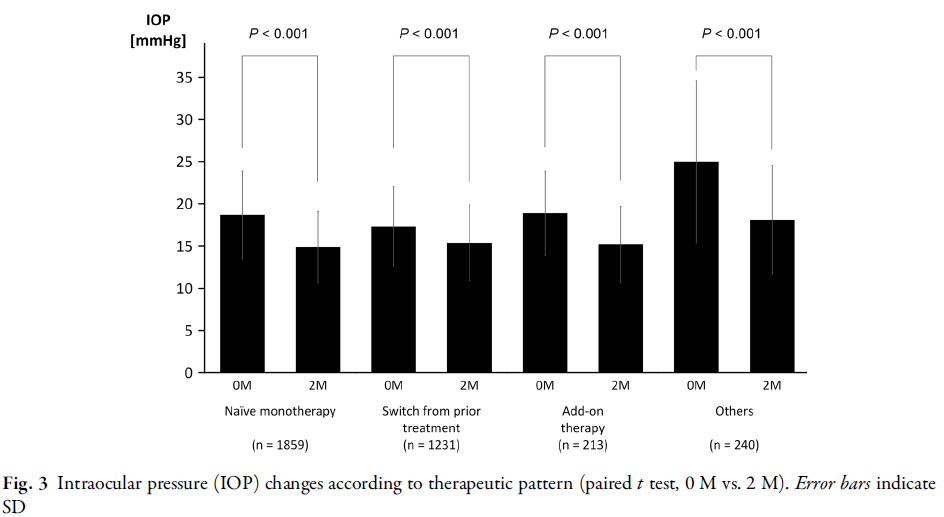
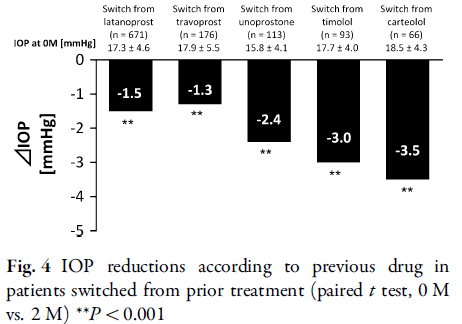
图2 继发性青光眼眼压(IOP)降低情况 按照治疗模式分析IOP的变化(图3和4)。首次单独治疗组IOP显著下降4.3 ± 4.0 mmHg,替换治疗组下降1.9 ± 3.5 mmHg,附加治疗组下降3.7 ± 4.1 mmHg。替换治疗组中,各类药物均出现IOP的显著下降,其中拉坦前列素下降1.5 ± 3.4 mmHg,曲伏前列素下降1.3 ± 3.7 mmHg,乌诺前列酮异丙酯下降2.4 ± 3.0 mmHg,噻吗洛尔下降3.0 ± 2.5 mmHg以及卡替洛尔下降3.5 ± 3.3 mmHg。
图3. 按治疗方案分类时的眼压(IOP)变化
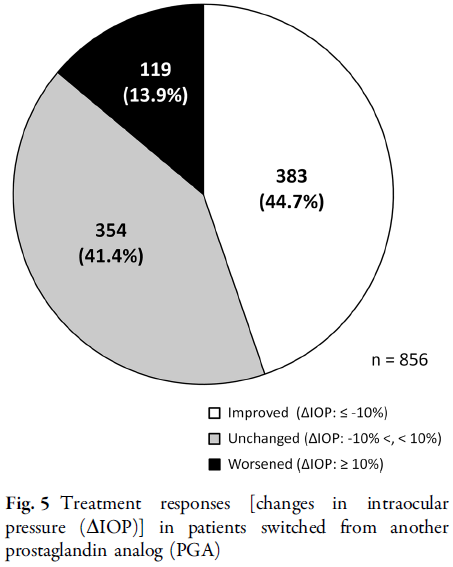
图4按既往用药分类的IOP降低情况 在从其他PGA改成他氟前列素的患者中,如将IOP降低≥10% 记为“改善”,IOP在10%之内波动记为“无变化”,IOP升高≥10%记为“加重”,则44.7%的患者为“改善”,41.4%的患者为“无变化”,13.9%的为“加重”(图5)。
图5从其他前列腺素类似物(PGA)改用本药后的治疗反应 0 4 客观结果评分 所有接受分析患者的平均结膜充血评分从1个月之后比基线值显著升高。若按治疗方案分析,首次单药治疗组和附加治疗组第1个月时分值显著增加,第2个月时该数值下降或呈下降趋势。替换治疗组显著降低(图6)。
图6 从0至2个月结膜充血评分情况 所有接受分析患者的平均角膜荧光素染色评分在第2个月时有所下降。若按治疗方案分析,首次单药治疗组和附加治疗组2个月时无显著改变。替换治疗组的分值显著下降(图7)。
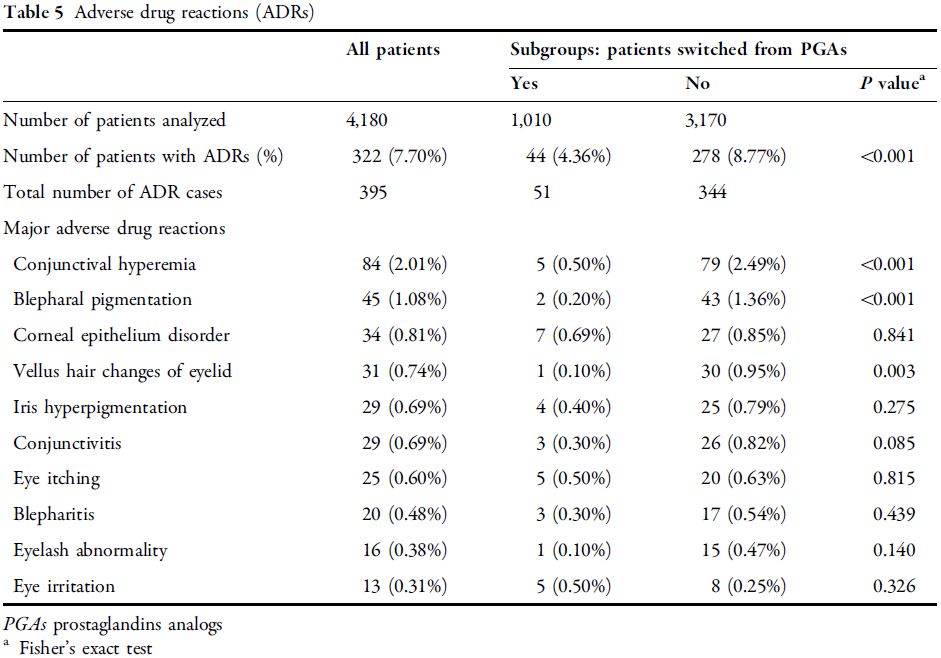
图7 从0至2个月角膜荧光素染色评分情况 0 5 不良药物反应 ADR的发生率为7.7%(表5),主要表现为结膜充血、眼睑色素沉着、角膜上皮异常、睑睫毛改变、虹膜色素增多、结膜炎和眼睛瘙痒。从其他PGA改用他氟前列素患者的ADR发生率(4.36%)显著低于未使用过PGA的患者(8.77%)。当按照ADR类型分析此类患者时发现,结膜充血、眼睑色素沉着、睑结膜改变发生率显著下降。
表5 药物不良反应 作者在结论中指出, 他氟前列素可显著降低常规临床工作中各类型青光眼和OH患者的IOP,且未出现安全性问题,他氟前列素对各种青光眼和OH的治疗模式均有效。 原文摘要 Advances in therapy, 2014, 31(4): 461-471. Prospective observational post-marketing study of tafluprost for glaucoma and ocular hypertension: short-term efficacy and safety. Kuwayama Y, Nomura A. Abstract INTRODUCTION This study investigated the intraocular pressure (IOP)-lowering effects and safety of tafluprost ophthalmic solution 0.0015% in actual clinical practice. METHODS We started a mandatory prospective 2-year observational study, which collected IOP, conjunctival hyperemia score, corneal staining score, and adverse event data from glaucoma and ocular hypertension (OH) patients not previously treated with tafluprost at 2, 12, and 24 months. This report analyzes the 2-month findings. RESULTS Of the 4,180 patients from 553 medical institutions in Japan, most patients had primary open-angle glaucoma (POAG, 38.1%) or normal-tension glaucoma (NTG, 44.2%). After 2 months of tafluprost administration, IOP was significantly reduced by 4.3 ± 5.2 mmHg in POAG, 2.4 ± 2.5 mmHg in NTG, 3.6 ± 5.3 mmHg in primary angle-closure glaucoma, 5.6 ± 7.1 mmHg in other types of glaucoma, and 5.3 ± 4.8 mmHg in OH. IOP was significantly reduced by 4.3 ± 4.0 mmHg in the naïve monotherapy group, 1.9 ± 3.5 mmHg in switching from prior treatment, and 3.7 ± 4.1 mmHg in the add-on therapy group. Among patients switched, the prostaglandin analog (PGA) latanoprost was the previous predominant drug (57.4%), followed by travoprost (13.8%). Significant IOP reductions were observed by 1.5 ± 3.4 mmHg in switching from latanoprost and 1.3 ± 3.7 mmHg in switching from travoprost. The conjunctival hyperemia score peaked at 1 month in the naïve monotherapy and add-on therapy groups, whereas it was significantly decreased in patients switched from another PGA. The corneal staining score showed no particular changes. Incidence of adverse drug reaction (ADR) was 7.70 % (322/4,180 patients), and all major ADRs involved the eyes or skin around the eyes. CONCLUSION Tafluprost showed significant IOP-lowering effects without any safety concerns in patients with various types of glaucoma and OH in daily clinical practice and tafluprost is highly effective in any therapeutic patterns. 并输入PMID号码 即可获取全文返回搜狐,查看更多 |
【本文地址】
今日新闻 |
推荐新闻 |